The Ontario government is spending $8.4-million to improve wait times and provide better access to pediatric mental health care in Durham Region.
The funding is part of the provincial government’s $330-million investment into pediatric services announced last summer.
The improvements include an eating disorder day treatment program at Ontario Shores Centre for Mental Health Sciences in Whitby.

The funding is also expected to reduce wait times for specialized mental health supports when people are released from treatment centres.
“That would probably be the biggest barrier to service is wait times,” said Janelle Haldenby, a child and youth counsellor at Lakeridge Health. “Having access to timely resources can really help especially when we know that early intervention and prevention is key.”
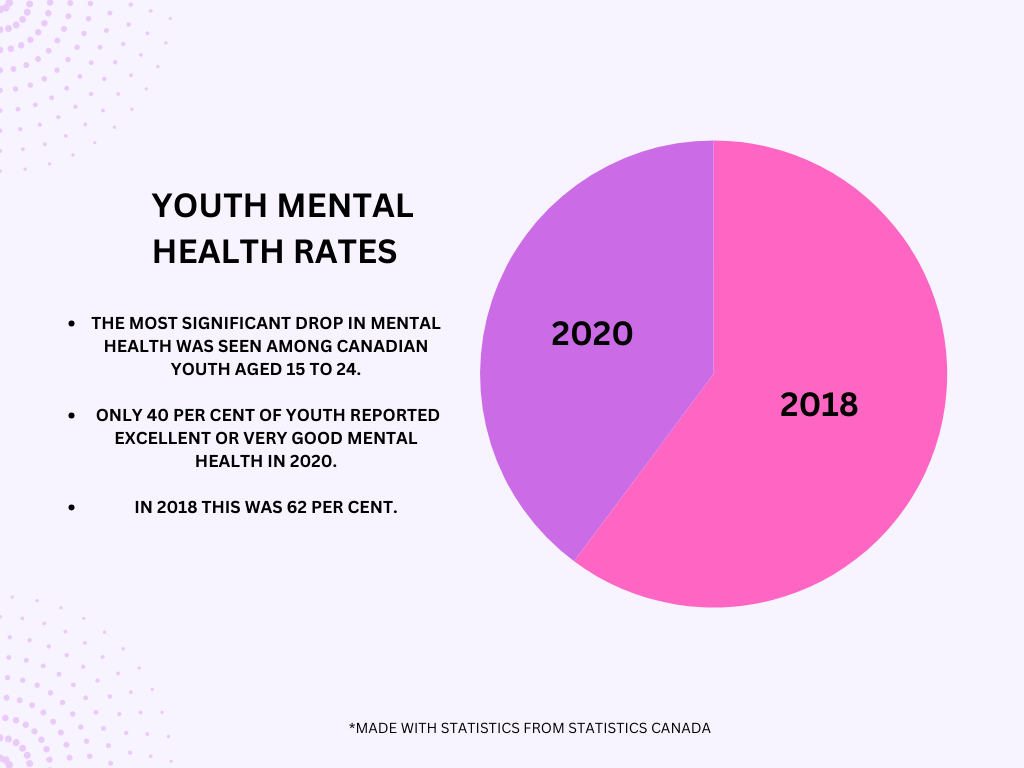
Nearly one in four hospitalizations for young people ages five to 24 were related to mental health in 2020, according to the Canadian Institute for Health Information.
Yet Children’s Mental Health Ontario says wait times range between nine months and two-and-a-half years.
Meanwhile, about 39 per cent of Ontario high-school students indicated a moderate-to-serious level of psychological distress in 2017, according to Canadian Association for Mental Health (CAMH). It says high demand for these services is causing prolonged waiting periods to access services.
However, Haldenby said the rise in youth struggling with their mental health is not the only factor contributing to this.
“There’s only so many child psychiatrists in Canada,” she said. “And people often don’t have the money to spend on private care like that unless they have [an] employee assistance program through their parent’s work or something like that… otherwise you go on the waitlist.”

According to Nour Hammami, a professor in the Department of Child and Youth Studies at Trent University, this investment will help reduce wait times since organizations can hire more people and properly address those who need help.
“That means there’s a tiny bit of less of a strain on health care workers,” said Hammami. “This is something that is much needed and they’ll be able to take a break, come back and sit with these children and youth.”
This investment also aims to address service gaps through ‘One Stop Talk’, a virtual walk-in mental health counselling service to aid in shortening these wait times.
She said these phone lines are important because they expand and address service since face-to-face consultations are not accessible to some.
“If you’re from Oshawa, commuting takes around over an hour by public transport to reach either Ontario resource or Grandview Children’s Center, and for many people, I wonder if this is accessible,” said Hammami.

She said phone lines can shorten wait times which gets people off waitlists, especially those who may not have time to commute to counselling meetings.
As this funding rolls out, some people are already looking towards the next steps for improving pediatric mental health services in the community.
“I think it’s a great first step, but the next steps would be how can we get equity deserving groups and marginalized groups, the services that they need as well,” said Hammami, “because those are the ones who really need them, so that would be what I hope for the next few years.”