Stomach issues and a talk with my family doctor lead to my first colonoscopy at 24-years-old.
It’s a young age to get one, and while it wasn’t specifically a screening for colorectal cancer, it would be a lie to say it wasn’t at the top of my mind. There’s a reason for this.
It’s become increasingly difficult to ignore the concern around cancer afflicting young people. A report published by Science in March, 2023 claimed an early form of colorectal cancer by the name of early-onset colorectal cancer (EOCRC) was rising to become “the leading cause of death in individuals aged 20 to 49 in the U.S. by 2030.”
As for Canada, a report published by Canadian Cancer Statics eight months later tells a different story, with colorectal cancer incidence and death rates declining “faster than the rate for any other cancer type,” and lung cancer mortality rate lowering.
In Canada, its recommended to begin screening for cancer at age 50, but change could be coming to other forms of cancer screening. The report, published in November 2023, also said cervical cancer is increasing at a “significant” rate.
According to Shannon Bourke, regional manager of cancer prevention and screening and the Indigenous cancer program at Lakeridge Health, cervical cancer will soon have a “way more effective” form of testing.
“In 2025, we’re hoping to see HPV testing come in instead of pap testing for cervical cancers,” she said.
Even though some forms of cancer are getting new forms of testing, she said it will be a while before Ontario lowers the screening age range for certain cancers, like lung cancer. According to Bourke, there are only four places for lung cancer screening in Ontario currently. Lakeridge Health is one of them.
“Lung cancer screening is one of our newer programs in Ontario, so it’s still kind of evolving and getting going,” Bourke said.
She also said their tag line “one in two doesn’t have to be you” means it’s important to get the necessary screening once you’re the recommended age and taking counteractive measures against cancer.
Some of these precautions include quitting smoking, sitting down for too long, and drinking alcohol.
In fact, Bourke said taking actions like quitting smoking, even after a cancer diagnosis, can reduce the risk of dying by 30 to 40 per cent, and a new report claims that one drink of alcohol is close to the mortality risk of one cigarette.
According to Christine Williams, Executive Vice President and Head of Implementation Science at the Ontario Institute for Cancer Research, one of the deciding factors in any change for cancer screening comes down to numbers, rather than the individual cases. She said the age cutoff for cancer screenings is decided at the population level and focused more on “big data” before anything else.
“Cancers mostly a disease of aging, so your likelihood of getting cancer increases with age,” she said. “Whatever the cause is, whether it’s sunlight, or genetic, or diet or whatever contributes to that, they accumulate over time.”

Williams said the risk of developing colorectal cancer below the age of 50 isn’t a cause for alarm yet, and the potential cost for health organizations and risk of false positives makes it a hard sell for health policies in Canada.
“If you get a false positive and have to go through additional testing, some of it is much more invasive, it’s certainly more costly,” she said.
However, she said some major changes do come from population level data, like what happened in the fall of this year. The Ontario government announced the age cutoff for breast cancer screening will go down from 50 to 40.
In the news release in October, Sylvia Jones, deputy premier and Minister of Health, said “nearly 12,000” women are diagnosed with breast cancer each year.
Williams says helping to lower the risk of a first diagnosis comes down to the right people getting the right message across. Infographics, like the one posted by ComPARe in 2019 are effective ways to communicate risks in a “digestible” fashion.
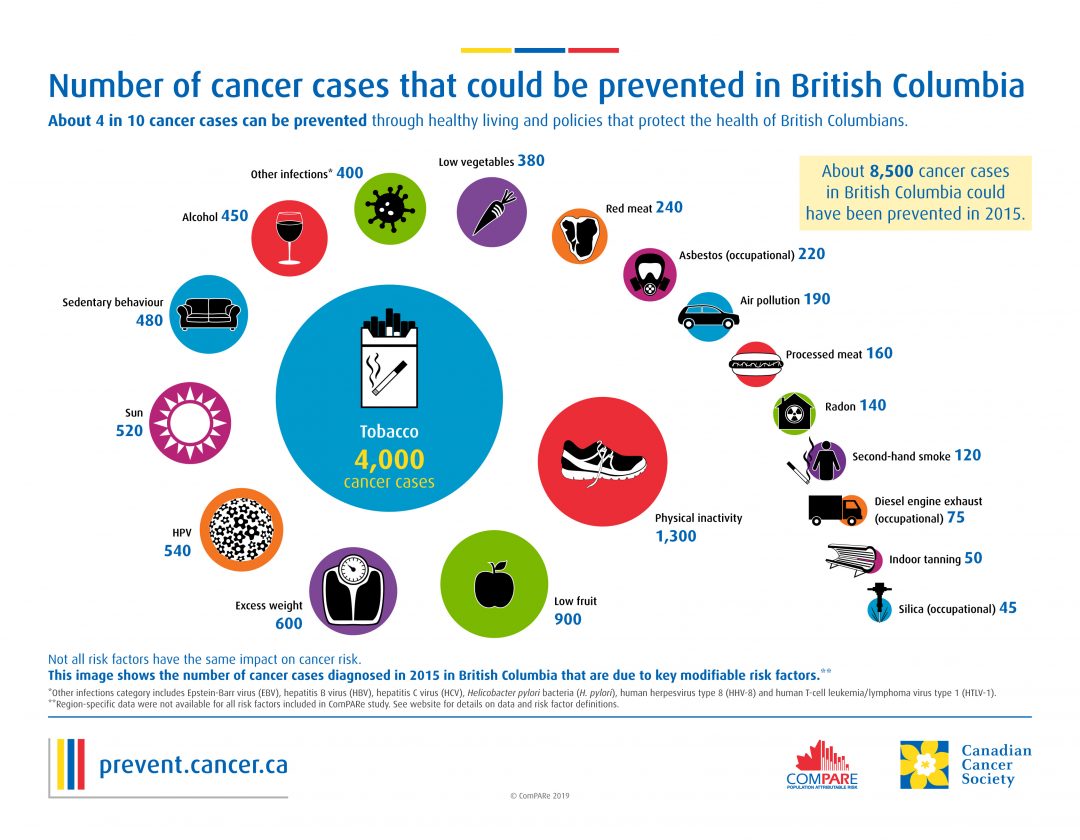
In the report, one of the highest attributed factors is a lack of fruit, and it claims 6,700 cancer cases could be prevented with sufficient fruit added to someone’s diet. Lack of vegetables isn’t far behind, accounting for 3,500 cases in the graphic.
Though some experts, such as Bourke, say it’s harder than it looks to eat healthy in the current economy.
Williams echoes the sentiment in the infographic, attributing some cancer causes to mental health and stress, a lack of physical activity, and dietary issues.
“Ultra processed foods are a concern for a lot of people,” she said, “our diet is changing and it’s changing the micro-environment of your gut.”
She says there’s speculation and some evidence that these changes in your gut are a leading factor for inflammation in the body, a condition she said is “mechanistically” linked to cancer.
According to Williams, it’s most important for young people to understand cancer, be proactive about living a healthy lifestyle, and to not ignore the warning signs. Something feeling off with your body is enough cause to go see your doctor and talk to them about how you’re feeling.
“One of the things that happens is that people ignore warning signs because they’re afraid of the diagnosis of cancer,” she said, “and I think that can be really counterproductive.”
Taking the steps to detect cancer earlier and getting the necessary screening makes treating cancer easier. By doing so, Williams said “you’re much more likely to have a good outcome and live a long and healthy life.”




