Medical Assistance in Dying (MAID) has been an option for Canadians with “grievous and irremediable” illnesses since 2016. On March 17, 2024, legal state-assisted suicide was supposed to be extended to include mental illness as the sole criterion for access.
The Liberal government has agreed that Canada is not ready to include mental illness as the sole condition for MAID. Still, Canadians need to put a permanent end to the notion that the state should be ending the lives of people whose only ailment is mental health-related.
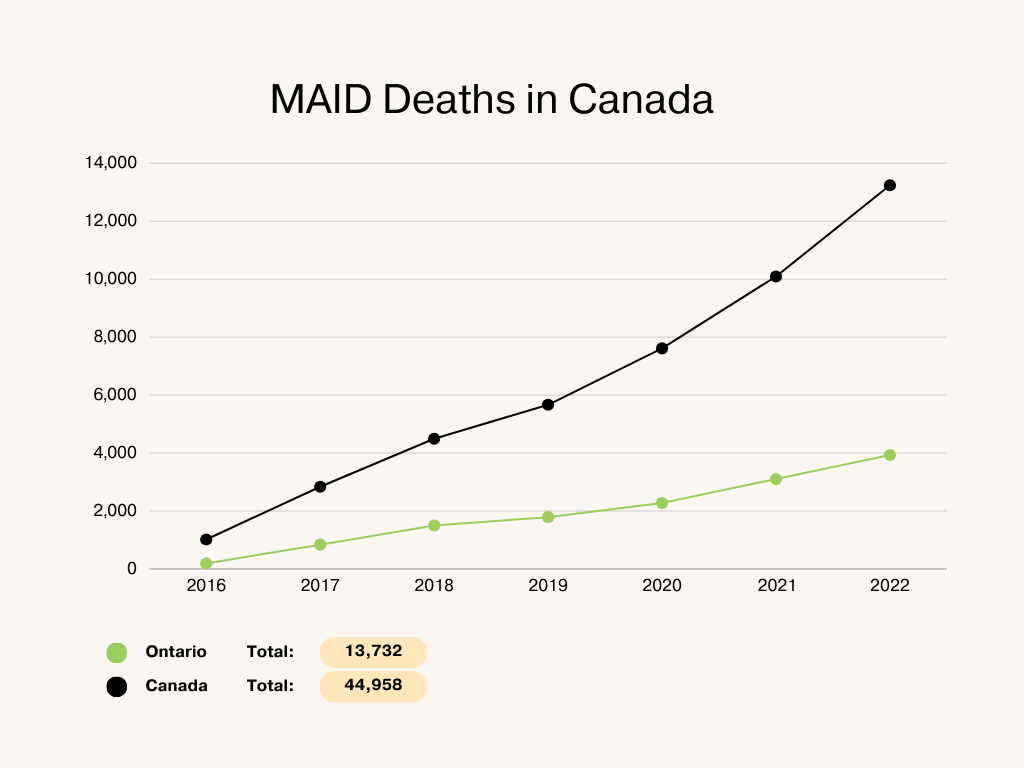
According to a poll conducted by the Angus Reid Institute, six out of ten Canadians support the MAID program as it is, which allows patients with severe, irremediable medical conditions that are worsening to access MAID; only three in ten support extending access to MAID based only on mental illness as a factor. Canada now has the highest MAID deaths in the world.
Unlike many physical illnesses, there are still so many things the medical community doesn’t know about mental illness and how to treat it. What works for one patient might not work for the next, and there is no way of knowing with certainty whether a patient will get better.
Dr. John Maher, a Neurologist in Barrie, Ont., has advocated for more safeguards to the MAID programs and the exclusion of mental health as a reason for access. He said estimating when someone gets better from mental illness is very different than estimating how long someone has to live with something like terminal cancer.
In a debate with fellow doctor Dr. Stefanie Green, Maher showed how wait times to access MAID are often shorter than those to access specialized health care and social support services. MAID took an average of 90 days to access, whereas veterans disability claims, for example, took an average of 273 days to process.
If these services were as accessible as MAID, some applicants to the MAID system might never have applied. Instead of investing time and money to extend the MAID system, the government should fortify mental health care in Canada.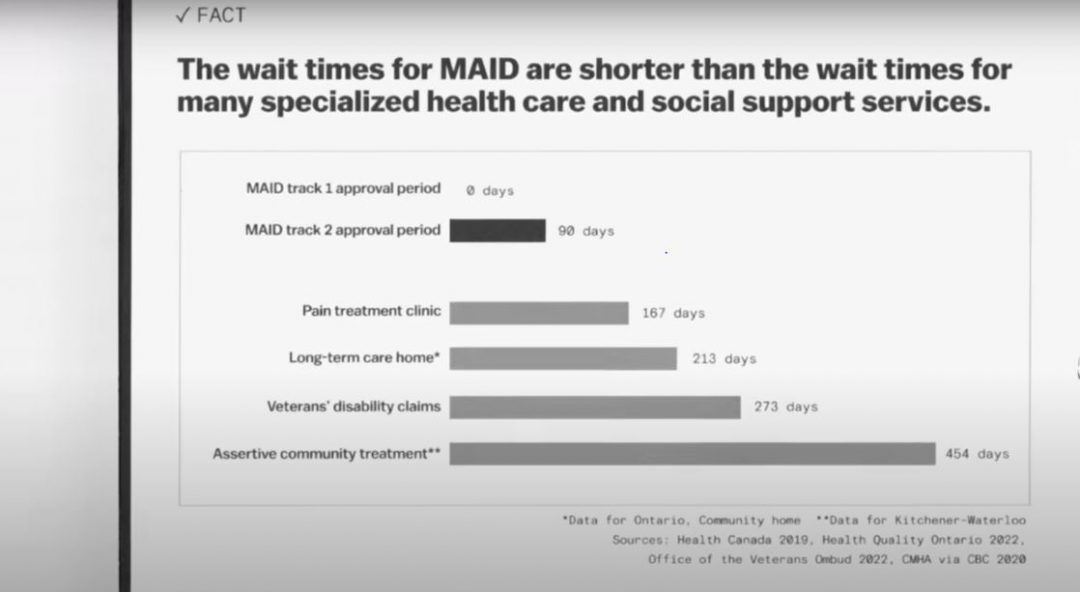
In the same debate, Green, author of “This is Assisted Dying,” points out that consensus is unnecessary to proceed with other medical treatments. In the case of MAID, two independent clinicians must agree that the patient’s condition is incurable for MAID to proceed. However, the lack of agreement among experts on the likelihood of recovery for many mental illnesses puts into question the accuracy with which decision-makers can predict that a patient is beyond saving.
To that point, extending access for people with mental illnesses might create a situation where patients give up on their healing and doctors will be less incentivized to find innovative ways of treating patients, knowing that MAID is always an option.
Maher has said that he’s had 30-year-old patients with “very treatable” mental illnesses ask to end their lives. How many people who either haven’t tried or can’t access treatments and support will seek out an end to their lives when there are other options?
In some cases, people are unable to access potentially life-affirming treatments and substances only available through Canada’s Special Access Program. Due to legislation, difficult-to-navigate bureaucracy, and a lack of staff trained in some treatments, access to MAID will become more accessible than access to life-saving medicines and therapy.
John Gilchrist of the patient advocacy group TheraPscil told the Chronicle last year that patients in their system had booked an “appointment to die using the MAID system, then tried psilocybin and cancelled their appointment.”
The fact that people who have signed up for MAID due to mental illness, in this case, end-of-life anxiety, have tried previously inaccessible treatments and decided to cancel their appointments is proof that for some people, what seems like an irremediable mental health condition can change with the correct supports.
Mental illness can also hamper a person’s ability to provide informed consent. One of the legal criteria for giving informed consent is competence. Mental illness can temporarily diminish a patient’s level of competence in this manner. While the majority of psychiatric patients maintain their capacity for decision-making, when people’s lives are in question, we shouldn’t take chances by taking the life of someone who is temporarily incapable of making a rational decision. Some tools will undoubtedly be used to detect patients’ ability to make those decisions. But mental illness being as complex as it is, there is no guarantee the patient’s capacity for making life-altering decisions will always be identified.
If the motion to include mental illness as a sole criterion for access to the MAID system is implemented, It will lead to unnecessary deaths. There is no way of telling if someone with a mental illness condition will improve. Mental illness hinders the judgment of people experiencing it, so they are often incapable of providing informed consent.
Instead of this addition to the MAID program, the government should focus on making sure all of our mental health supports and treatments are well funded, staffed and easily accessible, with little wait times for patients seeking potentially life-saving care.




