“I feel beyond hopeless. I’m tired of trying,” said Laura Rostron, a York Region patient with an eating disorder who was referred for care twice, in November and December 2024.
“Things are not great and the time frame that I’ve gotten for just the consultation alone is six-plus months,” she said.
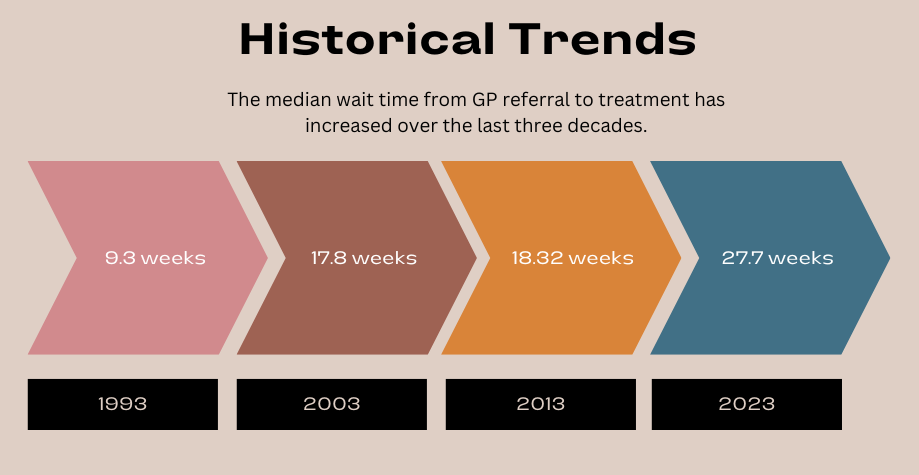
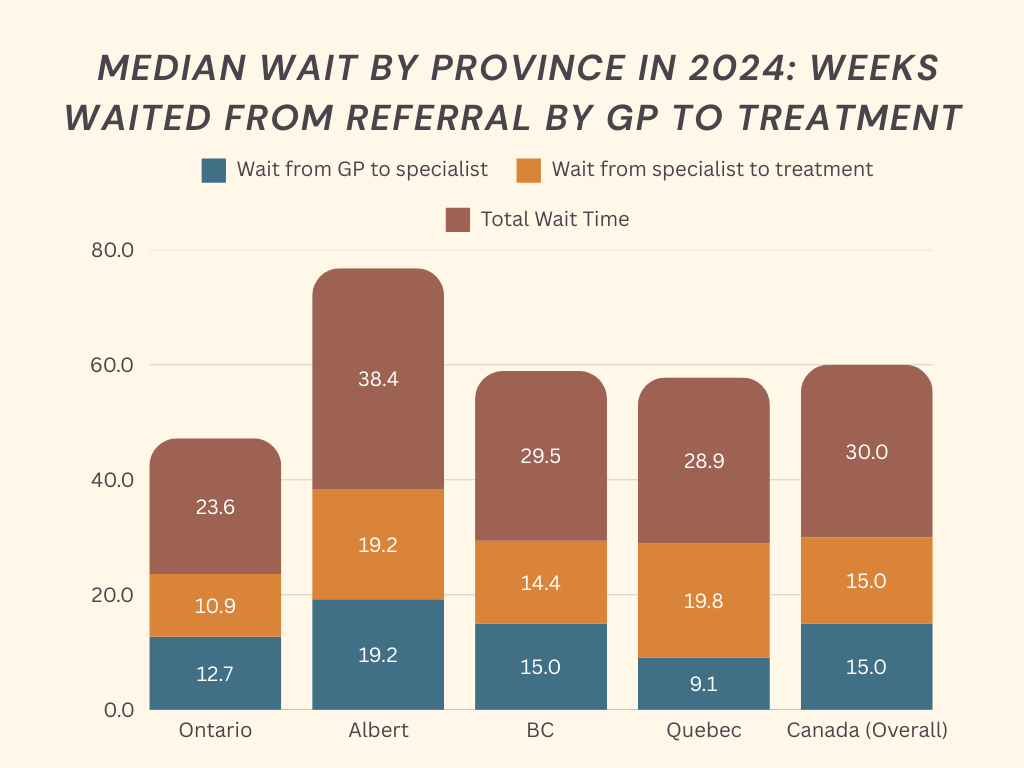
According to the Wait Times for Health Care in Canada 2024 Report, the median wait time between a general practitioner referral and treatment was 30 weeks, up from 27.7 weeks in 2023.
“The current state I’m in, like physically and mentally, is not good,” Rostron said.
“All I’m kind of encouraged to do is go to emergency if I need to and the downside is that if I go to emergency, they look at certain things and … they just send me home.”
Josephine Marchese, founder of NoMoreWaitLists.net, said wait times have increased in recent years, especially due to the COVID-19 pandemic which caused delays in surgeries and specialist consultations.
“As health-care systems recover from backlogs, some patients are still waiting 12 to 18 months for non-urgent procedures,” she said.
NoMoreWaitLists.net is an online service designed to connect patients with healthcare providers so they can receive timely care.
A Peterborough man, who wished to remain anonymous, has been on a waitlist for seven months for eye surgery due to keratoconus.
“They told me I had to get the surgery done before the end of 2024 to prevent further damage to my eyes and I still haven’t heard from the referral,” he said.
He has contacted the office three to four times since.
“They’ve resent the referral. They keep telling me it’s out of their hands because there’s only one location in the province that can do this surgery and I still don’t have anything,” he said. “I am forced to continue wearing glasses that are the incorrect prescription and further strain my eyes while waiting for this procedure.”
According to Benefits by Design data, in 2023, the median wait time in Canada from referral to specialist treatment was 27.7 weeks. Orthopedic surgery had the longest wait at 44.3 weeks, followed by gynecology (37.4), otolaryngology (35.2) and urology (31.1).
Marchese founded NoMoreWaitLists.net in memory of her father, who struggled to access health care in time. She said delayed medical care often leads to worsening health conditions, increased anxiety and a lower quality of life.
In some cases, prolonged waits result in costlier emergency interventions or, in severe situations, preventable deaths.
Wait times also have a serious impact on cancer patients, as delays can significantly worsen their chances of survival.
“Cancer can’t wait, and it doesn’t,” said Trevor Smith-Millar, communications manager of the Canadian Cancer Survivor Network.
Smith-Millar said cancer diagnoses dropped during the pandemic when many health-care services were paused.
“Those cancers could have been caught at stages 1 or 2, maybe. Now they’re being caught at stages 3 and 4 and so with this backlog that we’re currently going through not just in this province of Ontario but across Canada, that is significantly impacting cancer patients as a whole and making it more difficult to survive cancer,” said Smith-Millar.
With most people unable to access a family doctor and screening programs being limited, more cancers are being diagnosed at later stages, he added.
Marchese said staff shortages, high demand and limited resources are among the biggest contributors to long wait times in Ontario’s healthcare system.
Limited treatment slots and slow referral processes further strain access to timely care, she added.
Alanna Kong, research and campaigns coordinator at the Ontario Health Coalition, said wait times have not improved, particularly with the backlog of surgeries caused by COVID-19.
Kong referred to data obtained by Trillium Media, which reported that by September 2024, an average of 2,000 patients per day were waiting on stretchers in hospital hallways, the highest number recorded.
In 2016, before the Ford government was elected, 1.3 million Ontarians did not have a family doctor, according to Statistics Canada. By July 2024, that number had risen to 2.5 million, according to the Ontario College of Family Physicians, she referred. This marks a 92 per cent increase.
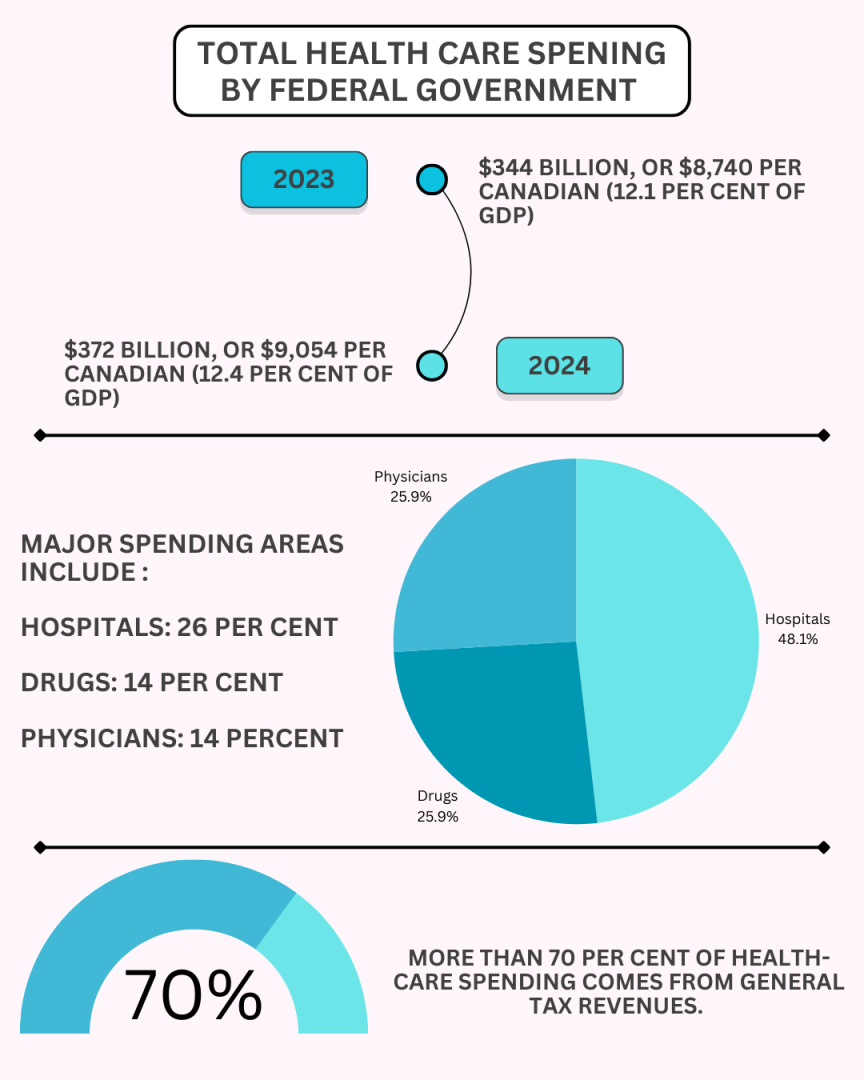
Marchese added that efforts to reduce wait times should include increased funding, telemedicine, AI-driven systems and private healthcare options.
Dr. Crystal Garvey, a professor in the collaborative BScN program at Durham College and Ontario Tech University, primarily in emergency and mental health nursing, said long wait times result from multiple factors.
“With regards to wait times in the institution … there’s a lot of compounding factors why we have these really long wait times. It really does start with the funding,” said Dr. Garvey, who has more than 20 years of nursing experience.
Dr. Garvey emphasized the need for education from the community to the government.
“People need to understand what services are allocated for and how to access them to be more effective and efficient in their care,” she said.
“Walk-in clinics are not obligated, nor will they for the most part, provide you referrals to specialists,” Garvey said.
Without a family doctor, patients often have no choice but to visit the emergency room, leading to high costs.
Kong also highlighted the issue of patients turning to emergency rooms due to a lack of family doctors.
“Their only option is to just go to an emergency department, so people have no choice but to go there to get things like a prescription that a family doctor or family practitioner should just be able to give you,” she said.
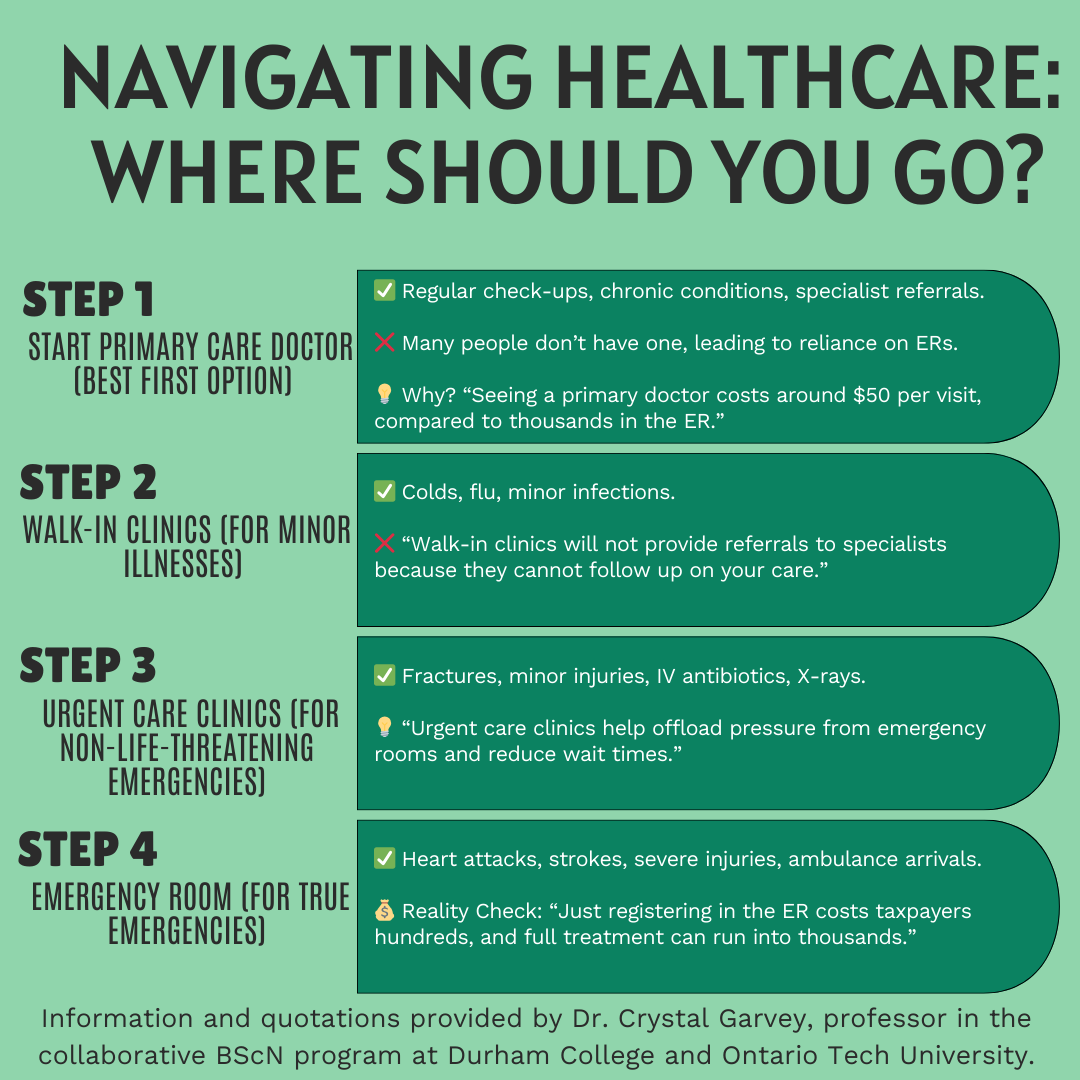
Urgent care clinics offer a better alternative, Garvey added.
“Urgent care clinics are another great resource for us to access, which will offload some of that burden from the emergency room,” she said.
She also highlighted the lack of public awareness.
“If the government were to take the time to do these little commercials about what is what and informing the community, I believe that would decrease some of those wait times,” she said.
Garvey said the situation is worse for people of colour.
“Think about all the evidence about wait times and the barriers to wait times just for the human being and now let’s add in the dimension of race, or you’re an immigrant, or you’re a person that wears a hijab or turban. All these things now compound your issue astronomically,” she said.
Garvey emphasized the importance of advocating for oneself.
“So if you’re going to your family doctor and you have a health issue that you’ve been navigating, go prepared and do your research before you go into the clinic. And this is why I say have somebody with you, because sometimes there’s power in numbers,” said Garvey.
Rostron said talking is one thing and funding is another.
“An action is required. Talk without action means nothing,” she said.