“At the time, I just wanted the pain to stop,” Chris Cull says, recalling the day he walked into his father’s hotel room and found him dead by suicide. His father had been suffering from Huntington’s disease, and that moment shattered Cull’s world
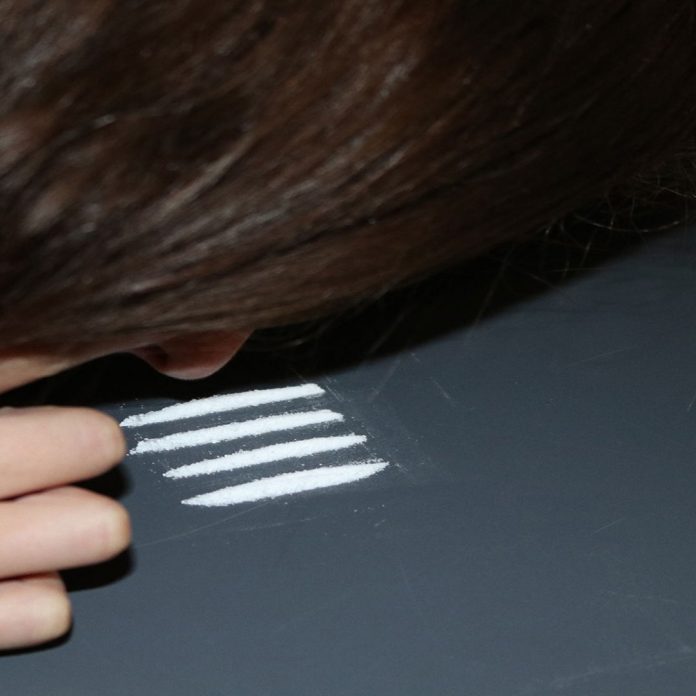
The grief was overwhelming and like many others grappling with trauma, he sought solace in opioids. What began as a way to numb his pain spiraled into a years-long addiction, costing him relationships, his home and his dignity.
Cull’s crisis extends beyond personal tragedy. Opioid addiction is a significant public health issue in Durham Region and across Canada.
According to the Durham Region Health Department, opioid-related emergency visits rose by 74 per cent from 2017 to 2020, and in 2020 alone, the region reported 91 opioid-related deaths.
The Ontario Drug Policy Research Network (ODPRN) highlights the urgency further, noting that opioid deaths across Ontario surged by 79 per cent during the COVID-19 pandemic. These statistics underscore the pervasiveness of the crisis and the urgent need for action at both local and national levels.
For many, addiction is not simply about physical dependency—it is deeply tied to trauma. Cull’s descent into substance abuse was driven by the grief of losing his father, a trauma so profound it pushed him to seek any form of escape.
“Addiction is more than a physical craving—it’s an emotional one,” he explains. His story mirrors a broader reality. Numerous studies, including those from Public Health Ontario, reveal that adverse childhood experiences, such as abuse, neglect, or the death of a loved one, significantly increase the likelihood of substance misuse.
In Cull’s view, the absence of community, purpose and goals exacerbates this vulnerability.
“If you lose any one of those things, it’s easy to fall into addiction,” he says.
His insight reflects the complex interplay between trauma and substance use, showing how deeply rooted personal pain can lead to life-altering consequences. These insights are echoed in research from the Canadian Centre on Substance Use and Addiction (CCSA), which emphasizes the need to address underlying emotional pain to prevent relapse.
In response to the growing crisis, the Canadian government has implemented various measures to combat opioid addiction. Nationally, harm reduction strategies such as supervised consumption sites and naloxone distribution have been expanded.
Naloxone, a medication that reverses opioid overdoses, has become widely available in public spaces, pharmacies and community centres. According to Public Health Ontario, thousands of naloxone kits have been distributed across the province, saving countless lives.
“Every time I share my story or help someone on their path to recovery, I know I’m saving a life,” Cull says.
Cull has worked with the Canadian Centre of Substance Abuse and Addiction (CCSA) on developing opioid prescribing guidelines to reduce the over-prescription of painkillers, a crucial factor in preventing addiction.
According to the Durham Region Health Department, 5,025 naloxone kits were distributed in the Durham Region in 2023.
In the Durham Region, Rapid Access Addiction Medicine (RAAM) clinics provide same-day support for individuals seeking treatment. Public Health Ontario emphasizes these clinics play an essential role in addressing the surge in opioid-related emergencies by offering immediate care and linking patients to long-term recovery services.
However, Cull stresses efforts must go further.
“Addressing addiction requires tackling the mental health crisis and affordability issues too,” he notes, highlighting the interconnectedness of social and economic factors in addiction.
Cull argues that a more holistic approach is needed—one that integrates mental health services, housing support and employment assistance to address the root causes of addiction.
Trauma is a known catalyst for substance use with research indicating up to 75 per cent of people with substance use disorders have experienced significant trauma, such as abuse, neglect or loss.
Despite the grim statistics, Cull’s journey toward recovery is one of resilience and hope. His turning point came during a seemingly trivial incident at his cashier job, where a customer threw a sign at him over a minor pricing dispute.
Physically scarred but emotionally awakened, Cull realized he needed to change. He quit his job and began methadone treatment, taking small but steady steps toward recovery.
“Recovery isn’t about a sudden transformation—it’s about doing a little better each day,” he says.

Today, Cull shares his story to inspire others, advocating for those struggling with addiction, and reminding them change is possible. His work includes public speaking engagements, mentorship and involvement in policy discussions to improve support for those in recovery.
Cull’s journey from addiction to advocacy underscores the power of perseverance. As he continues to work on various projects, including a forthcoming book and TED Talk, his message is clear: “You’d be surprised at how far you can go from a point you thought was the end.”
His story not only sheds light on the human toll of the opioid crisis but also offers a beacon of hope, illustrating that with support, purpose, and determination, recovery is always within reach.